Faced with the rise of “fake injectors” in aesthetic medicine, it becomes crucial to understand this alarming trend. These practices not only compromise patient safety, but also undermine confidence in the profession. This article explores the risks associated with these unqualified actors, and highlights the importance of proper training.
What are fake injectors?
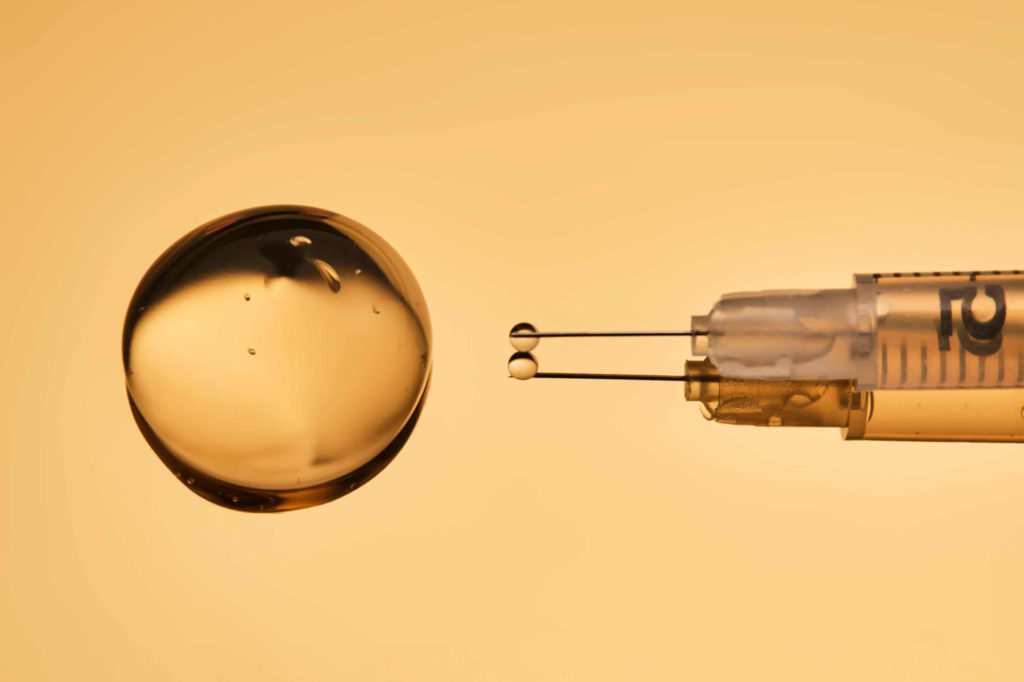
A “fake injector” is someone who injects dermal fillers without legal authorization or expertise. In recent years, we’ve seen an increasing number of offers, particularly on social networks, to have hyaluronic acid injected to increase the size of the lips, correct a bump on the nose or increase the size of the cheekbones. In short, to improve appearance, but above all to meet the beauty standards imposed by social networks. And in reality, aesthetic medicine is something completely different: it’s a global approach focused on appearance, but one that will take place over time, with support for patients and a notion of prevention and long-term care. The promise of “fake injectors” is often the opposite. It responds to an immediate, pressing, extreme demand to extrapolate its appearance. But if that were the only problem, we could say: everyone makes their own choices about the way they look. The real problem with “fake injectors” is obviously the risk to physical integrity, since the consequences of hyaluronic acid injections are potentially serious in terms of aesthetics and even function.
What does the law say?
Well, the law states that the use of skin-piercing injections for aesthetic purposes by beauticians and non-health professionals is illegal. It’s easy to see why you need a medical degree, or at least a diploma in supervised nursing. So that’s the first thing to ask if you want to have cosmetic injections. The second thing is training. This is exactly why SAMBA exists, to train healthcare professionals who wish to carry out aesthetic injections. They are trained not only in basic anatomical knowledge to prevent complications, but also to act correctly with a perfectly edited protocol, particularly in the case of intravascular injection of fillers leading to tissue ischemia. So it’s essential when you want to have cosmetic injection treatments to make sure that the practitioner, even if authorized by law, is properly trained in injection techniques.
Why is it dangerous?
Hyaluronic acid is a wonderful product, but even if it’s good quality, if it’s injected into a vessel, in this case a facial artery, it will clog the artery. It’s important to understand that all the tissues of the face – skin, muscle and fat – are vascularized, which means that as soon as you go under the skin, you can encounter an artery or vessel, and therefore potentially use a needle to enter this vessel and push in a filler that will block the vessel. This is what we call embolization: once the vessel is blocked, everything downstream will be acutely ischemic. This means more oxygen is delivered to downstream tissue.
The first consequence is a whitening of the skin corresponding to the vascular territory. Then, if there is no immediate intervention by the practitioner, a change to an inflammatory and ischemic state with skin that becomes red and then bluish (livedo). Finally, in the hours and days that follow, tissue necrosis occurs. Quite simply, the death of the fabric. So you end up with skin that turns black, putrefied, simply dead, and instead you have a hole, a loss of substance. If it’s the tip of the nose, you lose the tip of the nose; if it’s on the nasolabial fold, you have a scar; if it’s on the glabella, you have a scar. If, in addition, the injector pushes a large quantity of the product, it can travel up to the artery which, this time, feeds the eye’s retina and block this artery, leaving you with monocular blindness, i.e. blind in one eye. It’s over, you’ve had ischemic retinal necrosis and you’re blind in one eye for life, and that’s not a story or a fantasy. Theoretically, this is perfectly documented, since the facial artery joins the angular artery, which in turn is directly connected to the central retinal artery. But above all, all you have to do is go to the internet, and more specifically, if you want a reliable source, go to pubmed and type in “blindness filer” and you’ll see official publications, particularly in Asia, because there are a lot of injections in high-risk areas in Asia, of people going blind with hyaluronic acid injections in an artery. It is therefore extremely important to understand that a licensed and trained practitioner will be able to intervene rapidly if he or she observes an injection into a vessel. So there’s a risk for everyone, and where there’s a loss of chance is that if you’re faced with a “fake injector”, he won’t have the skills or the tools to handle the emergency.
The second risk is obviously linked to the products themselves. Practitioners who are authorized to inject dermal fillers on a regular and official basis can be considered to have products that meet the required standards and are therefore unlikely to have any product-related side-effects. The main side effect of the bad product is intolerance of the skin to the product, and therefore rejection in the form of inflammation and granuloma, which will leave balls under the skin that are very difficult to remove, or even impossible to remove, even surgically, because they are completely integrated into the skin tissue, the fat and even the ligaments and muscles of the face. Without going that far, you can simply end up with a post-injection infection if hygiene rules are not followed, which is often the case with “fake injectors”. Authorized healthcare professionals practice in regulated premises where they are bound by strict hygiene rules, whereas “fake injectors” go and do it in an apartment, in a basement, in places where minimum hygiene is not guaranteed. In short, it’s a matter of public health, a matter of your physical integrity, not to respond to the sometimes tempting sirens of “fake injectors”.
What to do if you are a victim
As you’ll have gathered, if there’s a complication with a “fake injector”, you’ll be kicked out, sometimes even physically threatened. I’ll leave you to enjoy some of the stories you’ll find on the networks or by typing into your search engine. The fake injectors are very reactive, often structured, and will reopen just a stone’s throw away, re-promote on social networks and re-inject new patients. It reopens, because, to be perfectly transparent, most of the time you won’t have any complications (except that the result is ugly). Even when you don’t know exactly what you’re doing, it’s fortunately extremely rare. But if you’re a victim, there’s no one left to take care of the emergency.
So what to do then? If, by chance, you have a medical acquaintance, you call him or her right away so that he or she can direct you. If it’s a SAMBA-trained aesthetic doctor, it’s bingo! He can (after he agrees) treat you as an absolute emergency for the problem of ischemia in particular. If not, go to the emergency room. Unfortunately, emergency departments are often not competent to deal with these problems, since they’re not something you learn in hospital, so you need to know how to describe the problem. Above all, emergency departments don’t have the miracle enzyme that immediately dilutes and dissolves hyaluronic acid, called hyaluronidase. Only aesthetic physicians and authorized personnel have the enzyme hyaluronidase in their practice or clinic. So first of all, you need to find a competent healthcare professional who can act quickly. The protocol for injecting hyaluronidase into the ischemic zone is simple: continuous mass injection with hour-by-hour monitoring for the first 12 hours. Then daily follow-up to see how the tissues are progressing, so of course if sight is at stake, that’s another problem. A retrobulbar injection must be carried out as a matter of urgency. Very few practitioners know how to perform it at SAMBA, so we’re going to run a course dedicated to this rather extreme type of injection, which can save a patient’s visual function.
In the case of infectious or inflammatory problems, there is no absolute urgency. Except for the infectious problem if it gets worse. So you need to go and see a doctor, explain what’s happened and treat a classic skin infection. You’ll also need to dissolve the product (which means going to a trained professional such as a SAMBA doctor). If you’re faced with the wrong product and you develop inflammation with granuloma, you’ll need to go to a specialist.
To sum up
First step: don’t go to a fake injector
The second step is to visit a licensed practitioner.
The third step is to go to trained staff (SAMBA is the best) in a facility that complies with strict hygiene rules, using top-quality products that have been tried and tested for a long time and have all the necessary marketing authorizations.
SO first :
Find out more! As for your practitioner’s qualifications, ask, for example, whether your doctor has undergone training or has a diploma such as SAMBA. If not, what was his training? Take a look at the SAMBA website to see what it’s like to have a complete training course, with theoretical knowledge and practical training to really master emergency situations. Find out what you need to know, just as you would for any other act of consumption. If everything is OK, you can calmly resort to aesthetic injection techniques which, when properly performed, produce extremely positive, long-lasting, harmonious results that respect everyone’s differences without being visible or shocking to those around you or yourself. In short, it’s a treatment that brings enormous satisfaction and well-being to patients.