Arterial embolization, a taboo subject rarely discussed, is a dreaded complication in aesthetic medicine during hyaluronic acid injections. This article looks back at an unpublished exchange of several clinical cases encountered by Drs Marie Nichanian-Broglia, Guilhem Poron, David Rousset and Clément Guyot, and highlights best practices for effectively managing these delicate situations.
What is embolization?
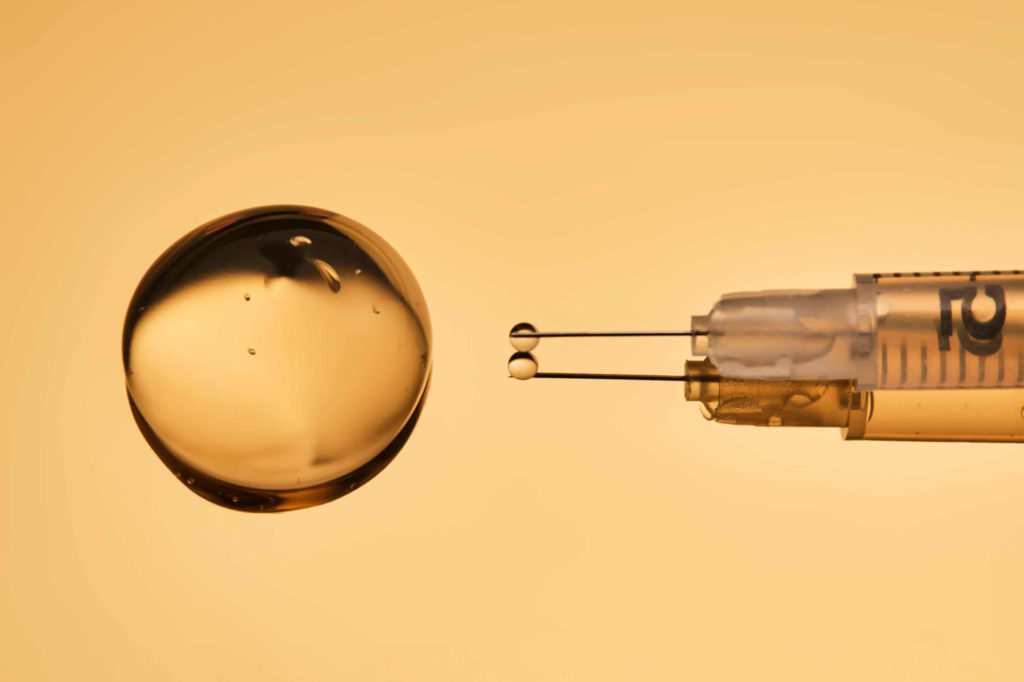
Embolization occurs when an injected product clogs an artery, causing ischemia. Although the risk is low, it requires rapid and appropriate treatment. The doctor’s training and experience can help reduce the risk of major complications.
Case studies: when embolization becomes a reality
Our doctors share a number of outstanding experiences:
- The case of Dr. Guyot : ” I injected hyaluronic acid into the nasolabial fold. I didn’t notice any immediate signs of ischemia, but the patient reported complications a few hours after the injection. The quantity I injected was 0.10 ml of a fairly dense hyaluronic acid. “
- Dr. Rousset’s case The embolization occurred following an injection of a poorly cross-linked hyaluronic acid into the glabella, which caused ischemia that remained localized, but which I was able to resolve quickly thanks to the administration of hyaluronidase.”
- The case of Dr. Nichanian-Broglia : ” I wanted to make a correction at the temple. The last bolus injected resulted in skin whitening, which required rapid intervention. I injected less than 0.05ml of hyaluronic acid. “
- Dr. Poron’s case : ” The embolization came after a medical rhinoplasty with a cannula. The situation was stressful, but I was able to manage it successfully. The amount I injected was between 0.05ml and 0.10ml. “
How to react to embolization?
1. Immediate identification of warning signals
Dr. Nichanian-Broglia reminds us of the importance of recognizing the first signs of embolization, such asskin blanching, unusual pain, ocular discomfort, livedo or vasculitis, and acting without delay. Hyaluronidase must be immediately available and injected in sufficient quantities. The doctor explains that lack of experience can sometimes be the reason why the result obtained is given priority over proper management of the accident. This reasoning leads some doctors to under-inject hyaluronidase, but ” it has no place in aesthetic medicine “, insists Dr. Nichanian-Broglia.
2. Never underestimate risk
Dr. Rousset reminds us that it is preferable to overtreat with hyaluronidase rather than minimize potential embolization, and that this requires the injection of a sufficient quantity of hyaluronidase. What’s more, rapid action helps avoid significant sequelae. Many scientific articles still mention the use of a cannula as a solution to avoid the risk of embolization. This statement is totally false, as in some cases it may even be much riskier to inject using a cannula. As Dr. Poron points out, ” there is no such thing as zero risk, and injecting the nasolabial fold is no less risky than injecting the glabella. ”
3. Apply protocols without hesitation
In the event of an embolic problem, it’s important to follow well-defined protocols, hence the importance of ongoing training. In this way, it’s essential to be well-equipped in all circumstances, and this includes a sufficient stock of hyaluronidase (4000 ui), whether in the office or, in the case of an emergency, during transport. When injecting, it’s important to act with delicacy and to respect the patient’s pain: ” The procedure should never be rushed,” insists Dr. Rousset.
4. Reassuring the patient
Only doctors who don’t inject don’t embolize. It’s therefore perfectly normal for such incidents to occur, but they can nevertheless seriously compromise the bond of trust established with the patient. For this reason, reassuring care and post-injection follow-up help to avoid stress and ensure optimal recovery. It’s important to make the patient understand that this is a problem that doctors are capable of dealing with. What’s more, education is also essential in patient management, with patients needing to be aware of symptoms in the event of a problem, so that they can contact their doctor as soon as possible. ” Aesthetic physicians have a responsibility to disseminate information. We can do incredible things with hyaluronic acid, but there’s always a risk, but if we’re well trained, we can achieve restitution ad integrum. “assures Dr. Poron.
Lessons learned:
- Continuing education: Mastering anatomy, tools (needle or cannula) and keeping up to date with the latest recommendations. Apply best practice recommendations to every injection throughout your career.
- Stress management: Remaining calm in the face of the unexpected to reassure the patient.
- Availability and follow-up: Ensure effective patient care and support throughout the process. Remain attentive to patient reactions and pain.
- Use hyaluronidase sparingly: don’t hesitate to administer sufficient quantities as soon as any doubt arises.
Conclusion
Embolization is a rare but very real complication in aesthetic medicine. With the right training, prompt management and a rigorous approach, it is possible to minimize the consequences and ensure patient safety. Indeed, the experiences shared by doctors remind us that patient safety must always take precedence over the aesthetic aspect. It’s interesting to note that most of the incidents shared in this article occurred during small corrections, often on the last bolus. A good reminder that “le mieux est l’ennemi du bien” (Perfect is the enemy of good), as Dr. Nichanian-Broglia says, explaining that it is sometimes preferable to be satisfied with the good result obtained, rather than seeking to improve it, at the risk of damaging it. As Dr. Poron reminds us, “there is no such thing as a risk-free zone, but with the right training and a rapid, appropriate response, you can restore skin integrity and avoid serious complications.