What does PRP mean?
Simply Platelet Rich Plasma. There’s no need to invent a marketing term to make it more chic: PRP is blood, your blood, centrifuged to recover the most interesting part – the platelets – concentrated in a small volume of plasma. It is this concentrate that is then reinjected where you want to stimulate repair or improve tissue quality.
A quick reminder for non-physicians who read the blog.
Blood is composed of :
- Plasma: translucent yellow liquid in which cells are immersed.
- Platelets
- Leukocytes or white blood cells
- Erythrocytes or red blood cells
The blood is centrifuged for a few minutes. It is the density of the various components that separates the plasma from the cells.
The platelets remain in the upper part of the tube in a plasma residue called
Platelet Rich Plasma.
It is more concentrated in platelets than in the initial plasma, because there are fewer quantities of plasma, some of which remains with the erythrocytes and leukocytes.
Why do we talk about Plasma Lift and Vampire Lift?
As is often the case, it’s the Americans who are the best at selling technology, and who coined the terms “plasma lift” or “vampire lift”.
It sounds better than PRP, it sells better. Plasma why not, Vampire why not, given that it bleeds when you do the injections, but lift I don’t really agree because I’ve never seen PRP lift a face.
It’s all about quality skin care. In short, it doesn’t really matter as long as you inject quality PRP correctly.
Indications for PRP
PRP is considered to be a tissue inducer. As such, its indications have multiplied. Basically, where you inject PRP, things get better, they repair, they improve, they produce tissue.
The most common indications are :
- In traumatology: intra-tendinous, intramuscular injection of PRP to improve healing
- In rheumatology/orthopedics for osteoarthritis, to improve healing.
- And of course in aesthetic medicine for skin rejuvenation and the fight against androgenic alopecia.
How is this done in practice?
Nothing could be simpler:
1. conventional blood sampling, butterfly needle puncture and sampling into a specific tube for PRP.
2. centrifugation
3. PRP recovery
4. distribution in syringes for intradermal injection
Mechanism of action of PRP
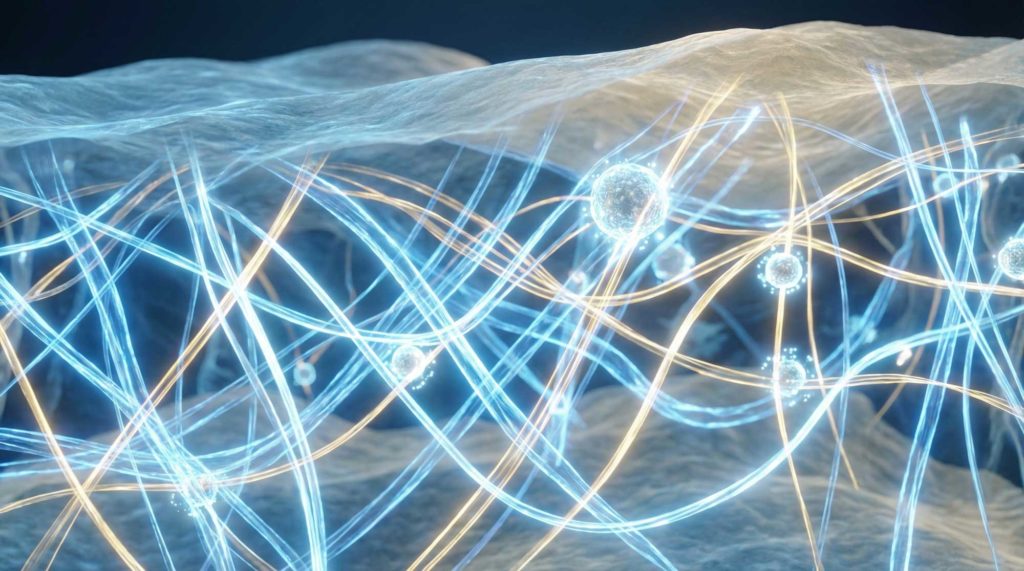
“PRP injected into target tissues causes a cascade reaction resulting in the production of various tissue growth factors.”
In particular, FGF: “fibroblast growth factor”, responsible for collagen and elastin production.
We could also mention the production of the following growth factors:
- PDGF (Platelet-Derived Growth Factor) ➝ stimulates proliferation of fibroblasts and mesenchymal cells, promotes angiogenesis and wound healing.
- VEGF (Vascular Endothelial Growth Factor) ➝ stimulates the formation of new blood vessels.
- TGF-β (Transforming Growth Factor beta) ➝ regulates collagen synthesis, fibroblast differentiation, modulates inflammation.
- EGF (Epidermal Growth Factor) ➝ promotes keratinocyte proliferation and re-epithelialization.
- IGF-1 (Insulin-like Growth Factor 1) ➝ stimulates muscle and bone regeneration, promotes anabolism.
- FGF-2 (Fibroblast Growth Factor 2) ➝ stimulates angiogenesis, cell proliferation and tissue regeneration.
PRP injection also induces the production of pro- and anti-inflammatory cytokines.
- IL-1β, IL-6, TNF-α (present in small quantities depending on the type of PRP) ➝ activate the initial inflammatory response required for wound healing.
- IL-4, IL-10 ➝ anti-inflammatory cytokines, limit the chronicity of inflammation and promote “clean” regeneration.
PRP injection also induces the production of complementary molecules:
- SDF-1 (Stromal Derived Factor 1) ➝ attracts stem and progenitor cells to the site of injury.
- MMPs and TIMPs (Matrix Metalloproteinases and their inhibitors) ➝ remodel the extracellular matrix.
- Serotonin, histamine, catecholamines ➝ modulate vascular permeability and pain.
PRP in aesthetic medicine
We have seen that injection of PRP into the target tissue leads to a cascade of production favorable to tissue stimulation and healing. In aesthetic medicine, the target tissue is the dermis.
PRP injected intradermally stimulates the production of FGF, which in turn stimulates fibroblast production of collagen and elastin.
PRP is therefore used in skin rejuvenation to improve skin quality.
- Micro-ridules
- Elasticity
- Brightness
- Balancing the bio-lipid film
- Prevention of dermatoporosis and photoaging
Which patients undergo PRP?
PRP at the aesthetic doctor’s
PRP is not authorized in all countries, as it is a blood-derived product.
As is often the case, it’s a case of the authorities regulating out of ignorance of safety processes and the risks involved.
In fact, apart from the risk of blood exposure inherent in any subcutaneous injection, PRP injections present very few risks for patients. An intra-vascular injection of PRP is ultimately a return to the source of the product injected.
Beware: in some PRP tubes, hyaluronic acid is added, notably for rheumatology and orthopedic indications. In such cases, the risk of intravascular thrombosis is clearly present.
Obviously, training in the sampling, centrifugation and injection process is essential. The basics have to be learned. But by following simple processes, it really is an easy-to-deliver and effective treatment.
I would add that, at the present time, an autologous treatment like PRP couldn’t be more “organic” or sustainable.
It would be desirable for the authorities to focus more on regulating cosmetic procedures carried out by unqualified individuals, who endanger the physical integrity of patients on a daily basis, and, conversely, to promote and encourage proper training for those eligible, as well as access for patients to this high-quality care.
What do patients say about PRP?
PRP is a subcutaneous skin quality treatment, so it’s more a matter of feeling and skin well-being than being truly quantifiable.
It’s not like IPL or Pico on spots or hyaluronic acid injections in the lips.
PRP is part of the therapeutic toolbox for long-term patient care, improving skin quality and preventing photoaging and dermatoporosis.
My patients are true PRP “fans” who have integrated it into their skin care routine.
I share this vision with my patients. PRP, at 3 sessions a year, seems to me to be a “game changer” for long-term skin quality.